Bilateral Oophorectomy and Salpingectomy: Comprehensive Insights

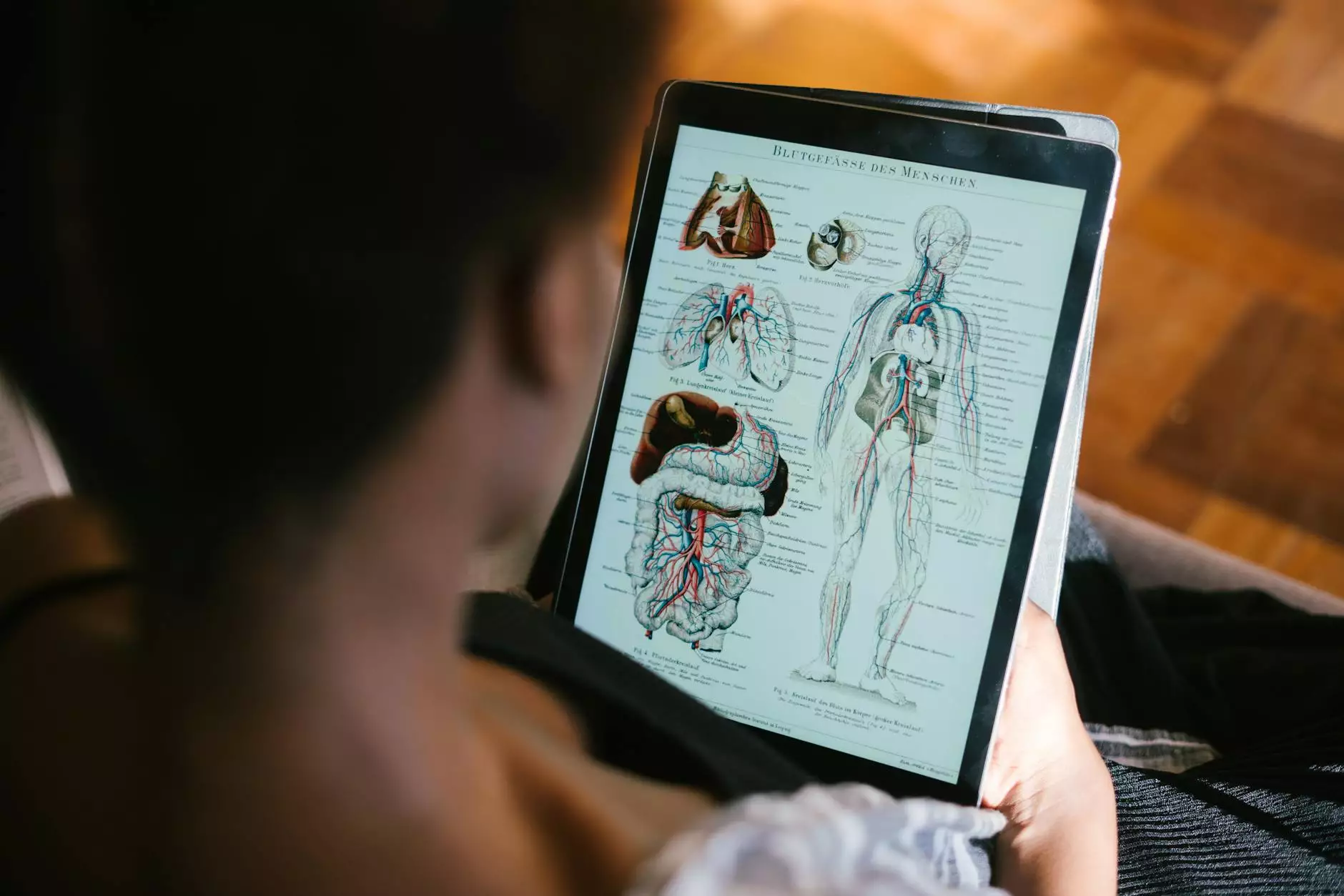
Introduction to Bilateral Oophorectomy and Salpingectomy
In the realm of gynecological health, surgical procedures play a crucial role in addressing various medical conditions. Among these procedures, bilateral oophorectomy and salpingectomy have garnered significant attention due to their implications in women's health, particularly relating to the prevention of malignancies and management of other reproductive issues.
Understanding the Definitions
Before delving deeper, it is essential to understand what these terms mean:
- Bilateral Oophorectomy: This surgical procedure involves the removal of both ovaries. It is often performed to treat conditions such as ovarian cysts, endometriosis, and certain types of cancers.
- Salpingectomy: This involves the surgical removal of one or both fallopian tubes. It can be done alone or in conjunction with oophorectomy and is often indicated for ectopic pregnancies, infections, or other pathological conditions.
Reasons for Performing Bilateral Oophorectomy and Salpingectomy
There are several reasons why a healthcare provider might recommend a bilateral oophorectomy and salpingectomy. These include:
- Cancer Prevention: Women with a high genetic risk for ovarian and breast cancer may opt for this surgery as a preventive measure.
- Treatment of Endometriosis: For patients suffering from severe endometriosis, the removal of ovaries and fallopian tubes can alleviate pain and prevent future complications.
- Recurrent Ovarian Cysts: Persistent and painful cysts that do not respond to fertility treatments may necessitate removal of the affected ovaries.
- Pelvic Inflammatory Disease (PID): Chronic infections can damage the reproductive organs, prompting the need for surgical intervention.
The Surgical Procedure Explained
Understanding how a bilateral oophorectomy and salpingectomy is performed can help demystify the process for patients. The procedure typically involves the following steps:
- Anesthesia: General anesthesia is administered to ensure the patient is unconscious and free of pain during the surgery.
- Incision: The surgeon makes an incision in the abdominal wall, which can vary in size based on the surgical technique (open surgery vs. laparoscopic). Laparoscopic surgery is less invasive and has a shorter recovery time.
- Removal of Ovaries and Tubes: Once inside, the surgeon carefully detaches the ovaries and fallopian tubes from surrounding tissues and blood vessels.
- Surgical Closure: After the removal, the surgeon closes the incisions with sutures or staples and applies dressing to the surgical sites.
Benefits of Bilateral Oophorectomy and Salpingectomy
The decision to undergo this surgery should be well-informed and based on an assessment of its numerous benefits:
- Reduction in Cancer Risk: By removing the ovaries and fallopian tubes, the risk of developing ovarian and certain types of breast cancers is significantly decreased.
- Pain Relief: Patients suffering from chronic pelvic pain due to endometriosis or other conditions often experience relief post-surgery.
- Improved Quality of Life: For many women, the elimination of painful cysts or the effects of endometriosis post-surgery leads to enhanced overall well-being.
Potential Risks and Considerations
Like any surgical procedure, there are inherent risks associated with a bilateral oophorectomy and salpingectomy. It is critical to have open discussions with your healthcare provider regarding these:
- Hormonal Changes: The removal of ovaries leads to a sudden decrease in hormone production, which can result in menopausal symptoms—hot flashes, mood swings, etc.
- Surgical Risks: General risks may include infection, bleeding, and complications related to anesthesia.
- Long-term Health Impact: Studies suggest a potential increased risk of cardiovascular disease and osteoporosis after oophorectomy, emphasizing the need for hormone replacement therapy in some cases.
Post-operative Care and Recovery
Recovery from a bilateral oophorectomy and salpingectomy varies among individuals. Factors such as surgical method and personal health play a significant role. Here are some general guidelines:
- Rest: Patients are advised to rest adequately and avoid strenuous activities for several weeks post-surgery.
- Pain Management: Medications are prescribed to manage pain and discomfort during recovery.
- Follow-Up Appointments: Regular follow-ups with the healthcare provider are essential to monitor recovery and address any complications.
Impact on Fertility
Understanding the impact of a bilateral oophorectomy and salpingectomy on fertility is crucial for individuals considering this procedure:
By removing both ovaries, the ability to conceive naturally is eliminated. Women should discuss fertility preservation options, such as egg freezing, prior to surgery if they desire children in the future.
Expert Insights from Dr. Seckin
Dr. Seckin, a leading figure in the field of obstetrics and gynecology, emphasizes the importance of personalized care when considering surgical interventions. According to Dr. Seckin:
"The decision to undergo a bilateral oophorectomy and salpingectomy should always be made collaboratively between the patient and their healthcare provider, taking into account the patient's medical history, risks, and future reproductive desires."
Conclusion: Making Informed Decisions
In conclusion, the bilateral oophorectomy and salpingectomy procedure offers significant benefits for women facing specific health challenges. However, it is crucial to weigh the potential risks and long-term implications carefully. Always consult with a trusted healthcare provider, like Dr. Seckin, to ensure an informed decision that aligns with your health goals.
References and Further Reading
For those interested in more detailed information regarding bilateral oophorectomy and salpingectomy, consider exploring the following resources:
- Dr. Seckin’s Official Website
- National Institutes of Health - Research and Publications
- American College of Obstetricians and Gynecologists